CAR T-cell therapy and engineered T-cell receptor (TCR) therapy are two types of cancer cell and gene therapy with similar characteristics.
CAR T-cell therapy broke through for blood cancer with the first FDA approval in 2017. KYMRIAH® (tisagenlecleucel) was approved for children and young adults with acute lymphoblastic leukemia with initial funding by Alliance for Cancer Gene Therapy.
CAR T-cell therapy and T-cell receptor therapy are not quite the same – although they are similar in many ways. Alliance for Cancer Gene Therapy explains how TCR therapies work and why they are different from the other well-known cancer cell and gene therapy.
What is CAR T-cell therapy?
CAR stands for chimeric antigen receptors, which are a genetic code enhancement to extracted T cells. This genetic code, a type of gene therapy, helps the T cells target cancer cells with a specific protein biomarker. One of the challenges with CAR T-cell therapies is the biomarker target can be in healthy tissue, meaning CAR T cells can attack and kill necessary healthy cells along with cancer cells.
There are already five CAR T-cell therapies approved for specific types of blood cancer. Aside from KYMRIAH, the other four are:
- YESCARTA® (axicabtagene ciloleucel) for non-Hodgkin lymphoma
- TESCARTUS® (brexucabtagene autoleucel) for mantel cell lymphoma
- BREYANZI® (lisocabtagene maraleucel) for types of non-Hodgkin lymphoma
- ABECMA® (idecabtagene vicleucel) for multiple myeloma
What is TCR therapy?
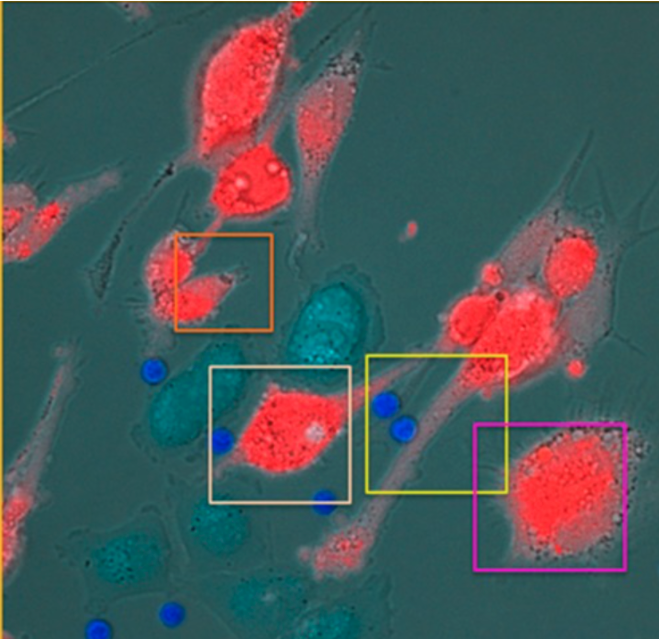
Engineered TCRs are similar to CAR T cells in being a next-generation cell therapy: T cells are extracted from a patient and enhanced in a lab to attach a receptor enabling them to attack the cancer cells. A major difference is engineered TCRs target specific proteins or antigens only linked to proteins that mark cancer cells.
T-cell receptor therapy accomplishes this by looking for a human leukocyte antigen (HLA), which is integral to presenting cancerous antigens to T cells. HLA is part of the major histocompatibility complex (MHC), which includes fragments of proteins called peptides.
When these peptides are from a cancerous protein, HLA presents them to the engineered T-cell receptors. The T cells then go on the attack, now alert to the abnormal peptide which is not present on healthy cells.
How KIMMTRAK treats uveal melanoma
The process explained above is similar to how bispecific fusion proteins like KIMMTRAK work. KIMMTRAK is a cell and gene therapy FDA-approved for uveal melanoma, which is a rare cancer of the eye.
One part of KIMMTRAK recognizes a marker that binds to a specific protein found in cells that produce melanin, including melanoma. The second part of the therapy recognizes a protein expressed by T cells, which are a type of immune cell. KIMMTRAK creates a bridge between melanoma cells and T cells allowing the immune system to attack and kill melanoma cells.
For KIMMTRAK, the marker targeted is HLA-A*02:01, which presents the melanoma antigen gp100 to T cells. gp100 is a lineage antigen expressed in melanoma cells. KIMMTRAK then binds the melanoma cells to T cells.
A scientific article published by the American Association for Cancer Research found that gp100 was only detectable on HLA-A*02:01-positive melanoma cells. The research supports using an engineered T-cell receptor for this specific HLA.
Alliance for Cancer Gene Therapy is a thought-leader in cancer cell and gene therapy research and treatment. Our mission includes funding development and increasing awareness of cell and gene therapies, including providing explanations of how each one works to slow or stop tumor growth and improve survival rates. The Alliance funded the initial science that led to CAR T-cell therapy FDA approvals for blood cancers, setting the stage for the wealth of cell and gene therapy research within hundreds of companies and institutions today.
With your financial contribution, we can improve the chances of other cancer cell and gene therapy approvals in the near future. Please join our Alliance today and do your part to fund the research that helps save lives.
Page sources.
- Immunocore announces FDA approval of KIMMTRAK® (tebentafusp-tebn) for the treatment of unresectable or metastatic uveal melanoma. Immunocore. Retrieved from: https://ir.immunocore.com/news-releases/news-release-details/immunocore-announces-fda-approval-kimmtrakr-tebentafusp-tebn/. Accessed: 01/27/2022.
- Abstract 2271: Tebentafusp recognition of melanoma cells is restricted by HLA-A0201 presentation of a gp100 peptide. American Association for Cancer Research. Retrieved from: https://cancerres.aacrjournals.org/content/80/16_Supplement/2271. Accessed: 01/27/2022.



