
Alliance for Cancer Gene Therapy (ACGT) is committed to advancing the science of cancer cell and gene therapy to transform cancer treatment and improve the outcome for patients.
This commitment involves funding groundbreaking cell and gene therapy research, starting with finding bold and innovative scientists devoted to approaching cancer research and treatment in unique ways.
Brian Brown, PhD, has one of the more unique and innovative approaches to aiding the immune system through cell and gene therapy. Dr. Brown, of the Icahn School of Medicine at Mount Sinai, is using grant funding from ACGT to use one immune cell to target another immune cell, albeit one that can protect tumors. His work was the highlight of an article published on Mount Sinai’s website.
What are macrophages?
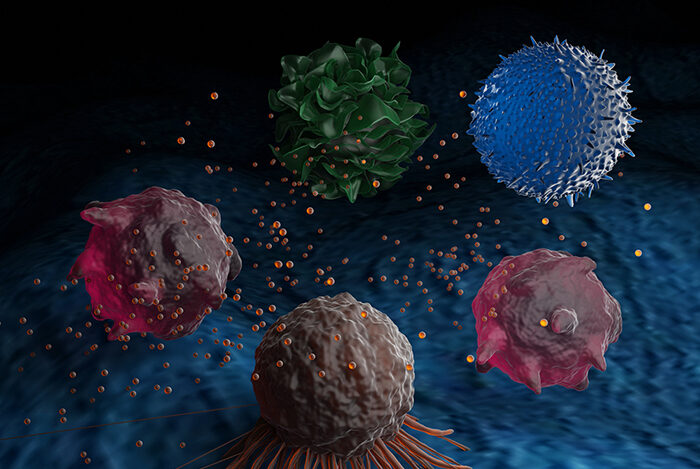
Dr. Brown’s research and development of a new therapy involves targeting an immune cell called macrophages. Macrophages are a type of immune system cell that cancer twists in its favor.
Macrophages help tumors grow by blocking T cells, another immune system cell, from infiltrating solid tumors. Macrophages also prevent CAR T cells, a type of cell and gene therapy, from penetrating solid tumors.
Dr. Brown’s approach is to engineer CAR T cells to target these macrophage cells and make tumors more vulnerable to immune response.
Explaining CAR T-cell therapy
CAR T cells are laboratory-engineered versions of T cells. Doctors remove T cells from the patient’s bloodstream and send them to a laboratory for genetic enhancements. The removed T cells receive a gene, which adds a special protein receptor. This receptor directs the T cells to attack cancer cells expressing an associated protein.
CAR T-cell therapy is a groundbreaking cell and gene therapy to treat blood cancers like leukemia, lymphoma and multiple myeloma. The U.S. Food and Drug Administration (FDA) approved the first CAR T-cell therapy in 2017 – which was developed thanks to ACGT funding. The FDA has approved several more CAR T-cell therapies since then to treat blood cancers.
Creating CAR T cells to kill macrophages
The presence of macrophages diminishes CAR T cells’ ability to target solid tumors. However, macrophages also express unique proteins that can be the target of CAR T-cell therapy.
Dr. Brown’s research led to developing a cell and gene therapy that targets macrophages. Once the CAR T cells engage with macrophages, they activate and attempt to kill the cell.
When put to the test, the macrophage-targeting CAR T cells performed well. According to the Mount Sinai article, the macrophage therapy “reduced the number of tumor macrophages, shrunk the tumors, and extended (the) survival” of mice with ovarian cancer, lung cancer or pancreatic cancer.
The killing of tumor macrophages made the mice’s cancer cells vulnerable to immune cells. The macrophage-killing CAR T cells also released a molecule (cytokine interferon-gamma) that stimulates an anti-cancer immune response.
“Our initial goal was just to use the CAR T cells to kill the immunosuppressive macrophages, but we discovered they were also boosting tumor immunity by releasing this powerful immune-boosting molecule. It was a one-two punch from this single treatment.” — Brian Brown, PhD, ACGT Research Fellow
What’s next for targeting tumor macrophages with cell and gene therapy?
The next step for the development of Dr. Brown’s research is to create human versions of the macrophage-specific CAR T-cell therapy. Once this is accomplished, the novel cell and gene therapy may advance to a clinical trial for solid tumors.
Alliance for Cancer Gene Therapy is thrilled to see this progress from Dr. Brown – an example of ACGT’s mission put to action. The scientist’s research is leading to a cancer cell and gene therapy that may be able to shrink ovarian, lung and pancreatic cancer tumors – progress driven by ACGT’s funding and donor support.
Progress like Dr. Brown’s at Mount Sinai is only possible thanks to donor support. Please donate to support cell and gene therapy research during the holiday season. Your generosity will help end 2022 on a strong note and put us closer to funding another research program that may lead to significant progress in the fight against cancer.
We’d also like you to sign up for ACGT’s email communications. We’ll deliver the latest news in cancer cell and gene therapy to your inbox.
Page sources
- Targeting One Type of Immune Cell With Another Slows Cancer Growth in Preclinical Studies. Mount Sinai. Retrieved from: https://www.mountsinai.org/about/newsroom/2022/targeting-one-type-of-immune-cell-with-another-slows-cancer-growth-in-preclinical-studies. Accessed: 11/15/2022.



