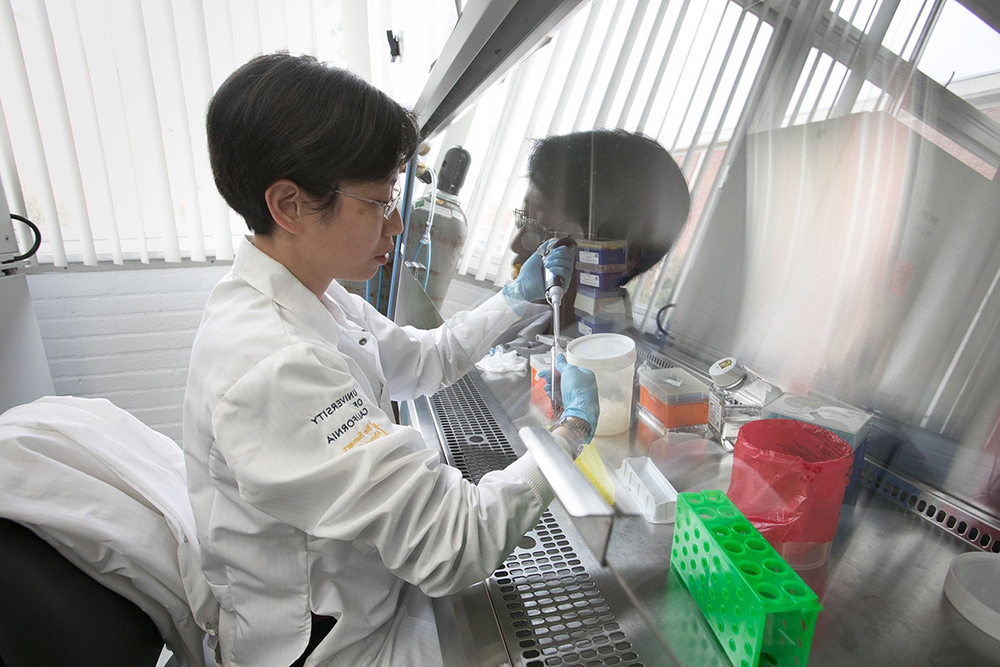
Yvonne Chen, PhD (University of California, Los Angeles), is an ACGT Research Fellow and a leading scientist in cancer cell and gene therapy. She is a professor of microbiology, immunology and molecular genetics and a professor of chemical and biomolecular engineering at UCLA.
She’s also codirector of the Jonsson Comprehensive Cancer Center Tumor Immunology Program and a researcher at the Parker Institute for Cancer Immunotherapy.
Dr. Chen‘s research interests include applying synthetic biology and biomolecular engineering techniques to develop robust cell-based therapies for otherwise-intractable diseases.
Bispecific CAR T cells developed in Dr. Chen’s laboratory are being tested in clinical trials, and she’s currently developing next-generation CAR T cells with enhanced specificity, reduced toxicity and the ability to overcome tumor-associated immunosuppression.
Dr. Chen received funding from ACGT in 2015 to study CAR T-cell engineering mechanics to help scientists design effective CAR T cells to target different cancerous proteins, and therefore, different types of cancer. This research led to the development of CAR T cells capable of targeting two proteins expressed by lymphoma cells, and in 2019 she started a phase 1 clinical trial testing the engineered T cells.
What or who inspired you to focus your research on immunology, specifically cell and gene therapy?
Dr. Chen: I was fortunate to stumble into the field of T-cell engineering as a chemical engineering PhD student at the California Institute of Technology. In a collaborative project with Dr. Michael Jensen, who was at City of Hope at the time, I worked on engineering ribozyme switches that could regulate cytokine expression in T cells to control T-cell proliferation. The CAR T-cell therapy field bloomed into wider recognition as I finished my PhD, and the academic freedom I had as a junior fellow in the Harvard Society of Fellows allowed me to focus on T-cell engineering and eventually build my laboratory at UCLA in this area despite not having been an immunologist by training.
When you were a young investigator, you received an ACGT Research Grant for a project that has since expanded and translated into clinical trials at a biotech company. Can you tell us a little about the translational path from starting your lab to launching clinical trials for patients?
Dr. Chen: The CD19/CD20 bispecific CAR T-cell therapy was the very first CAR engineering project I worked on. As a relatively young investigator, I found it challenging to know whether a technology we had developed would be worthy of clinical translation, and starting a clinical trial that is unlikely to generate publications for many years was a difficult decision for a pre-tenured faculty in an engineering department. However, with the encouragement and support of senior colleagues, I decided that therapies are only useful insofar as they can benefit patients, so we took the plunge into preparations and fundraising for the clinical trial. We were very fortunate to have received generous support from the Parker Institute for Cancer Immunotherapy to carry out the clinical trial, and we continue to treat patients in need of this therapy.
What did receiving the ACGT Research Grant mean for you and for your career?
Dr. Chen: The ACGT Young Investigator Award in Cell and Gene Therapy for Cancer was one of the first major grant awards I received. In addition to the financial resources that enabled us to explore new research topics, the recognition sent the message that my young research group was working on important questions that are worthy of support. ACGT’s vote of confidence meant a lot not only to me but also to members of my lab, and I believe it had a long-term effect on our group’s ability and motivation to keep pursuing projects that aim to bring real benefits to patients.
Cell and gene therapies had breakthroughs in treating blood cancers, specifically CAR T-cell therapies, and scientists like you are currently working to accomplish similar progress in solid tumors. How are CAR T-cell therapies being re-engineered to be effective in solid tumors?
Dr. Chen: A wide variety of strategies are currently being pursued, ranging from CRISPR screens aimed at identifying genes to knock in or knock out to increasing T-cell fitness to identifying additives during T-cell manufacturing that will optimize the quality of T-cell therapies. I personally believe that CAR T cells need to be able to adjust to and modify the tumor microenvironment to overcome challenges with solid tumors, and my group is working on combination strategies to achieve that goal.
Where do you see the field of cell and gene therapy going in the next five years, and what are some of the major opportunities for bringing therapies to patients?
Dr. Chen: Developments in cell and gene therapy aim to increase efficacy and reduce cost for patients. Promising approaches include the optimization of the manufacturing process to shorten wait times and potentially enhance T-cell fitness, the continued evaluation of allogeneic cell therapies that can provide off-the-shelf products, and the development of in vivo therapies (cells modified while still in the patient’s body) that bypass ex vivo processing entirely. Each of these approaches face challenges, but I am optimistic in the field’s ability to overcome technical obstacles. I also think ever-evolving techniques that enable us to gain a deeper understanding of immune-cell biology will eventually shed light on how best to engineer therapeutic cells to achieve robust efficacy while ensuring patient safety.



