For years, scientists needed one or two weeks to turn a patient’s normal T cells into enhanced cancer fighters known as CAR T cells.
Penn Medicine doctors and researchers weren’t satisfied with this norm, so they shortened the window extraordinarily – to within 24 hours.
“While traditional manufacturing approaches used to create CAR T cells that take several days to weeks continue to work for patients with ‘liquid’ cancers such as leukemia, there is still a significant need to reduce the time and cost of producing these complex therapies. Building on our research from 2018 that reduced the standard manufacturing approach to three days, and now to less than 24 hours, the manufacturing method reported in this study is a testament to the potential to innovate and improve the production of CAR T-cell therapies for the benefit of more patients.” — Michael Milone, MD, PhD, Penn Medicine researcher
Science behind CAR T-cell therapy
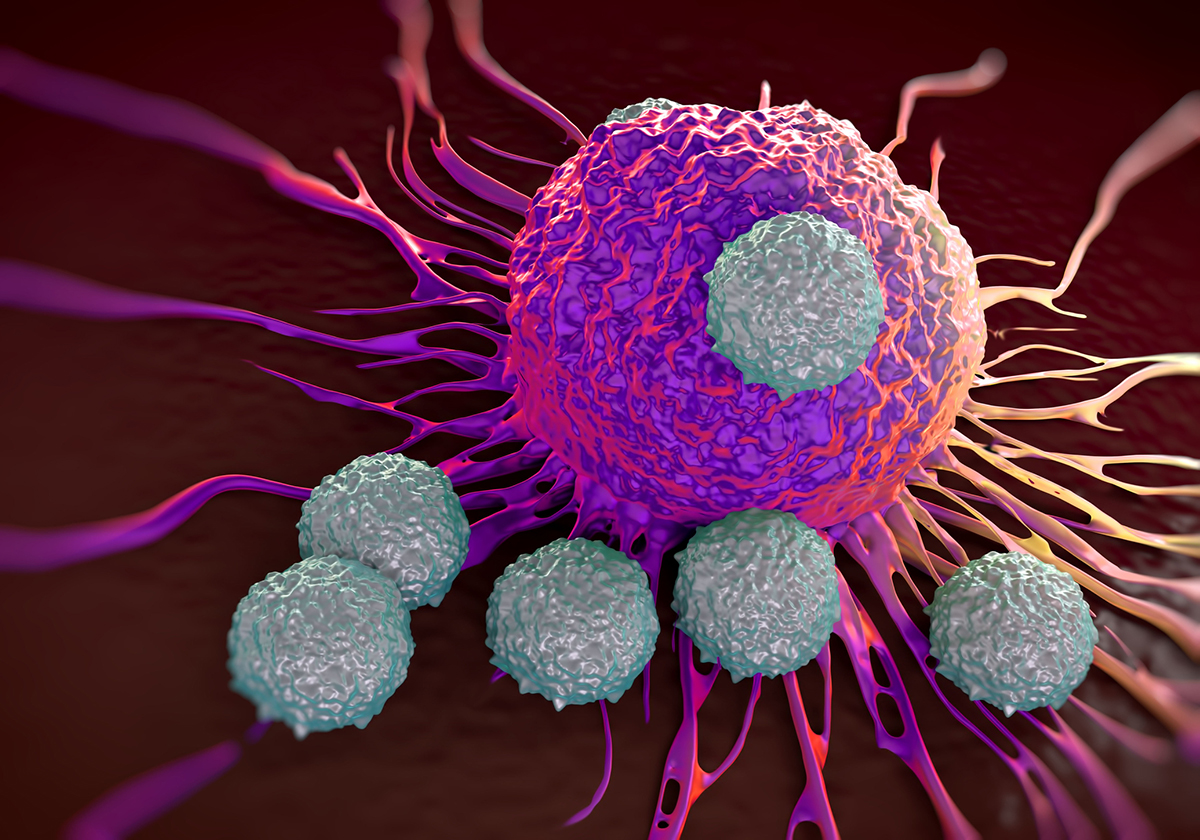
CAR T-cell therapy is one of the exciting cancer cell and gene therapies gaining support and recognition. CAR T cells are laboratory-enhanced versions of a patient’s original T cells. Doctors draw a patient’s blood and separate T cells, which are sent to a laboratory. Scientists add a chimeric antigen receptor (CAR) to the surface of the cells.
The new receptor includes a gene that teaches the cell to target a specific protein expressed on the patient’s cancer cells. The CAR T cells are infused back into the patient’s body, where they quickly go on the offense against the cancer cells comprising the tumor.
The new cells also replicate, which leads to a larger population of cancer-destroying CAR T cells than was originally provided to the patient. This phenomenon also creates a “living drug” which continues to replicate and persist for weeks, months or even years, preventing the defeated cancer from returning.
CAR T-cell obstacles
One of the obstacles for creating effective CAR T cells is the length of time the cells are outside of the body. Penn Medicine researchers reported the T cells may lose their ability to replicate, which is essential to creating a long-lasting therapy.
The traditional length of time for creating CAR T cells causes another obstacle: disease progression. The more time T cells spend in the laboratory receiving the necessary enhancements, the more time the cancer has to grow and spread inside the body, possibly to a level beyond the CAR T cells’ control.
How Penn Medicine cut the time to create CAR T cells

Usually, scientists take up to two weeks to replicate the CAR T cells and provide the patient’s immune system with an initial supply of the new cells. This time period is used to expand the CAR T-cell population adequately.
However, Penn Medicine researchers learned that the age-old cliché of quality over quantity pertained to CAR T-cell therapy.
Using animal models as tests, the scientists realized a smaller number of high-quality CAR T cells is superior to a higher number of lower-quality cells. Since the amount of time the cells are outside the body can affect their quality, the researchers realized shortening the time was critical.
Penn Medicine researchers also shortened the creation time in how they deliver the CAR gene to the T cells. The scientists used lentiviral vectors, which are from the human immunodeficiency virus (HIV) but cannot transmit HIV to the patient. Lentiviral vectors can transfer genes to cells without needing an activation, which CAR T cells traditionally require.
Penn Medicine’s use of this method expedited the manufacturing process without sacrificing the T cells’ potency. The scientists can now create effective CAR T cells within a day, possibly opening up other opportunities for simplifying the process.
“This innovative approach is remarkable in that it may be able to help patients who might otherwise not be able to benefit from CAR T-cell therapy, such as those with rapidly progressing cancer, due to significant time currently needed to generate these therapies. Efficient reprogramming of T cells with a CAR in as little as 24 hours in a more simplified manufacturing process without T-cell activation or extensive culture outside the body also offers the possibility of expanding where and when these therapies are produced. Not only might it improve the production capacity of centralized manufacturing facilities, but if simple and consistent enough, it might be possible to produce these therapies locally near the patient, which could be tantamount to addressing the many logistical challenges that impede delivery of this effective therapy especially in resource-poor environments.” — Saba Ghassemi, PhD, Penn Medicine researcher
Researchers at cancer centers across the U.S. are working to create more effective CAR T-cell therapies and more streamlined processes for delivering CAR T cells to patients. Alliance for Cancer Gene Therapy continues to identify and fund critical cancer research via donations, from people like you, to advance the discovery of cures.
100% of your financial support today will go to funding cancer research programs from the brightest scientists. Please donate today to join our Alliance and help us win the fight against cancer.
Page sources
- Penn Researchers Shorten Manufacturing Time for CAR T Cell Therapy. Penn Medicine. Retrieved from: https://www.pennmedicine.org/news/news-releases/2022/march/penn-researchers-shorten-manufacturing-time-for-car-t-cell-therapy. Accessed: 04/04/2022.



