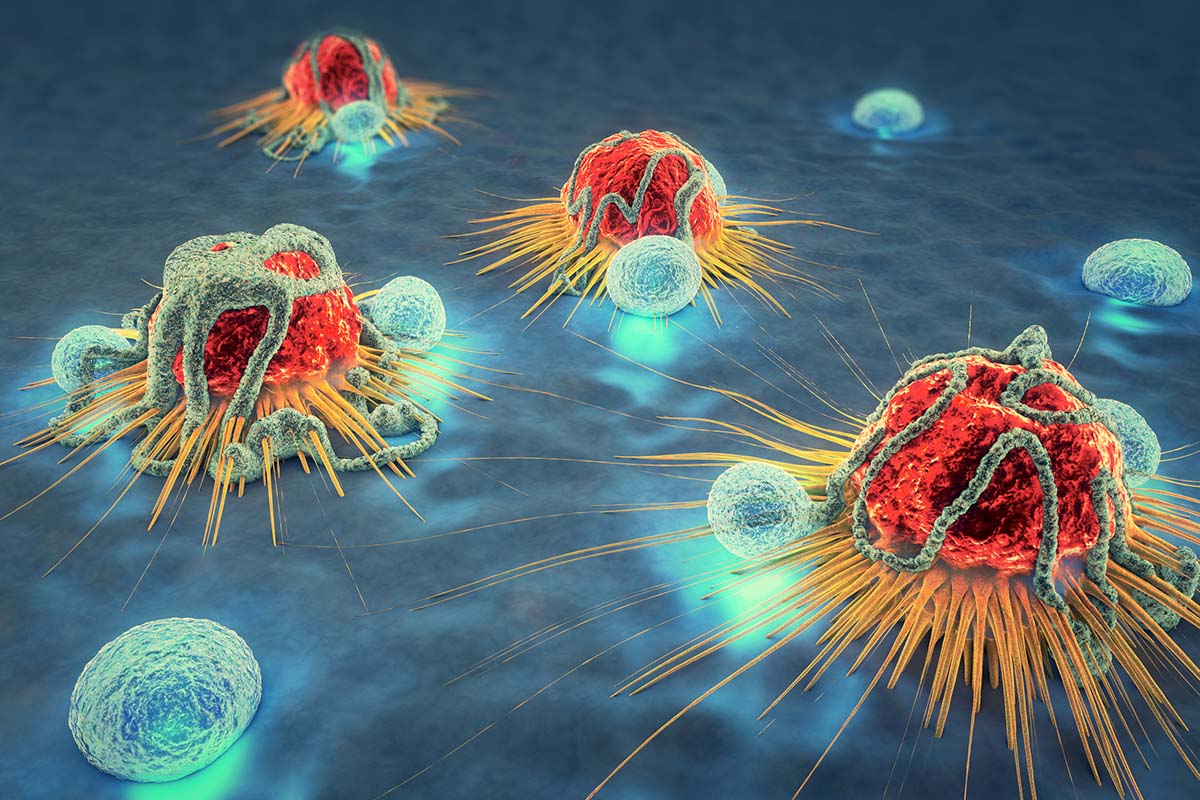
A major part of cancer cell and gene therapy is modifying immune cells to make them capable of killing cancer cells. Most immune cells need genetic alterations to prepare them for the confrontation with resistant tumors.
However, some immune cells may already be strong enough to do this job without modifications. These cells are called tumor-infiltrating lymphocytes. Is there a way to hone in on these cells and amplify their importance in the battle against cancer?
On Feb. 17, 2024, the U.S. Food and Drug Administration (FDA) approved the first tumor-infiltrating lymphocytes (TIL) therapy for cancer when it granted accelerated approval to Amtagvi (brand name of lifileucel) for people with unresectable or metastatic melanoma who were previously treated with a PD-1 blocking antibody, and if BRAF V600-positive, a BRAF inhibitor with or without a MEK inhibitor.
Alliance for Cancer Gene Therapy has published a guide to tumor-infiltrating lymphocytes and TIL therapy, including some of the latest developments in using it to treat solid tumors. If you’d like to learn more about Alliance for Cancer Gene Therapy, please visit our “Who We Are” page to see why our mission is focused on advancing cell and gene therapy research and development to transform cancer treatment.
What are tumor-infiltrating lymphocytes?
Tumor-infiltrating lymphocytes, or TILs for short, are white blood cells made in bone marrow that have migrated from the blood to the tumor. These immune cells have proven they’re able to seek out cancer neoantigens, which are fragments of mutated intracellular proteins presented on the surface of cancer cells. Additionally, they’ve successfully penetrated tumor cells and began chipping away at cancer.
TILs can be T cells or B cells, and they are candidates for transformation into a cancer therapy called TIL therapy.
What is TIL therapy?
TIL therapy is a cancer cell therapy that gives patients more tumor-infiltrating lymphocytes capable of destroying their tumors. People with cancer usually have TILs naturally penetrating their tumors, but not enough to destroy the disease. The cells also become exhausted and ineffective over time.
Scientists create TIL therapies by collecting a piece of the patient’s tumor and separating TILs from the tumor sample. The cells are then sent to a laboratory where they’re multiplied. The new TILs are returned to the patient’s bloodstream to continue attacking tumors in much larger numbers.
When the new TILs are re-infused into patients, they possess the same tumor-infiltrating traits as the original immune cells.
TIL therapy is a “bespoke” cancer therapy, which means it is made specifically for each patient rather than mass-produced for many patients (like chemotherapy). This is because TIL therapy is made from the patient’s own immune cells, possessing characteristics to fight that patient’s unique cancer.
Comparing TIL therapy and CAR T-cell therapy
TIL therapy is similar in some ways to another type of cell and gene therapy, CAR T-cell therapy. Both use the patient’s own immune cells to fight cancer.
The main difference is CAR T-cell therapy, short for chimeric antigen receptor T-cell therapy, requires scientists to genetically modify T cells in a lab to make them more proficient against cancer. The FDA has approved six CAR T-cell therapies for various types of blood cancers. None have yet worked consistently or safely for solid tumors, though.
One of the main reasons for this slower progress in solid tumors is CAR T-cell therapies need help attacking cancer. The CAR is a protein receptor added to the T cells genetically that directs them to search for cancer cells with the associated protein.
Blood cancer cells often have proteins that are not on healthy cells, which is why CAR T-cell therapy has been effective for these types of cancer. They can easily be engineered to search for proteins unique to the disease. Solid tumors usually have different cell types and share proteins with healthy tissue, making the development of effective CAR T-cell therapies much more challenging.
TIL therapy uses T cells that are already winning the battle against cancer. Rather than modifying these cells genetically, scientists simply have to expand their numbers so that the immune system has more cells adept at infiltrating tumors. This type of cancer cell therapy is promising since it doesn’t start from ground zero in the fight against cancer.
Using TIL therapy to treat cancer
Since TIL therapy uses cells that are already gaining ground in the battle with cancer, this type of cell therapy holds potential against solid tumors.
Amer Zureikat, MD, FACS, of the University of Pittsburgh School of Medicine, is an ACGT Research Fellow. He’s using grant funding from ACGT to explore using TIL therapy for pancreatic cancer. There are close to 60,000 new cases of pancreatic cancer in the U.S. each year, and the 5-year survival rate is a dismal 11%, which is the main reason why new therapeutic options like TIL therapy are needed to help patients.
Using TIL therapy for melanoma
Evident by the FDA approval of Amtagvi in 2024, TIL therapy has great potential as a solid-tumor cell therapy for melanoma, a type of skin cancer diagnosed in close to 100,000 people in the U.S. each year. TIL therapy has resulted in complete remission for 10%-20% of melanoma patients in clinical trials. Michael Lotze, MD, chair of ACGT’s Scientific Advisory Council, published the data and called it “practice-changing results.”
According to an article in the medical journal Nature, the TIL therapy Amtagvi was approved on the heels of a clinical trial in which there was a 31.5% anti-tumor response rate among 73 people with melanoma. Three patients had complete responses and 43.5% of the positive responses lasted for at least 12 months.
Tumor-infiltrating lymphocytes was the featured therapy of a recent melanoma clinical trial in the Netherlands, as reported by NBC News and other outlets. The results were presented at the European Society of Medical Oncology Congress in Paris, on Sept. 10, 2022.
In the clinical study, 168 patients with metastatic melanoma received either TIL therapy or the current standard treatment, an immunotherapy drug called ipilimumab given to patients who do not respond to first-line treatment.
TIL therapy impressively outperformed ipilimumab in the trial:
- 20% of patients receiving TIL therapy had a complete response, meaning their melanoma tumors disappeared.
- Only 7% of patients receiving ipilimumab had a complete response.
- The median survival from TIL therapy is more than two years, while ipilimumab led to a median survival of 1.5 years.
Using TIL therapy for other types of cancer
Melanoma is not the only solid tumor cancer that could be treated with TIL therapy. According to the article published in Nature, this cell therapy is currently in a phase 2 clinical trial for non-small-cell lung cancer and other clinical trials for various types of solid tumors.
Next steps in supporting further TIL therapy development
The FDA approval of Amtagvi and the news from clinical trials are evidence that TIL therapy has potential for solid tumors. It’s also evidence that the scientific community is inching closer to finding cures for cancer. Gaining official approval for use of TIL therapy for melanoma is a major step forward – and could save many lives.
Now is the time to keep the momentum going. ACGT asks you to join our Alliance of scientists, patients, biotech leaders and donors. The last group is the most important, as none of ACGT’s funding of innovative research programs would be possible without the support of our donors.
Please donate today to help ACGT support TIL therapy researchers and others who believe in cell and gene therapy as a potential cure for cancer. If you’ve enjoyed reading this latest news about cell and gene therapy, sign up for our monthly email newsletter to receive more updates directly to your inbox about this emerging field of cancer treatment.
Page sources
- New cell-based therapy for melanoma more effective than existing treatment, trial finds. NBC News. Retrieved from: https://www.nbcnews.com/health/cancer/new-cell-based-therapy-melanoma-effective-existing-treatment-trial-fin-rcna46935. Accessed: 09/14/2022.
- Efficacy of adoptive therapy with tumor-infiltrating lymphocytes and recombinant interleukin-2 in advanced cutaneous melanoma: a systematic review and meta-analysis. Annals of Oncology. Retrieved from: https://www.annalsofoncology.org/article/S0923-7534(20)32553-9/fulltext. Accessed: 10/03/2022.
- FDA grants accelerated approval to lifileucel for unresectable or metastatic melanoma. U.S. Food and Drug Administration. Retrieved from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-lifileucel-unresectable-or-metastatic-melanoma. Accessed: 02/20/2024.
- FDA approves first tumour-infiltrating lymphocyte (TIL) therapy, bolstering hopes for cell therapies in solid cancers. Nature. Retrieved from: https://www.nature.com/articles/d41573-024-00035-1. Accessed: 02/20/2024.



