One of the questions facing researchers is how to make CAR T-cell therapy safer and more effective as a treatment for solid tumors.
The answer might be having more control – specifically, remote control – over the CAR T cells.
Crystal Mackall, MD, a member of ACGT’s Scientific Advisory Council, designed a way to turn CAR T cells on and off while they’re in the body. She and others at Stanford University tested the method – called “remote-controlled CAR T-cell therapy – in mice with cancer. The results were excellent, and the goal is to begin a clinical trial for patients within the next two years.
“We’ve created a ‘remote-controlled’ CAR-T therapy that is tunable for each patient,” Dr. Mackall said in an article posted on the Stanford Medicine website. “These modified CAR-T cells are not only safer but they are also more potent and more versatile than the original CAR-T cells. It’s a pretty sophisticated system.”
CAR T-cell therapy: A living drug
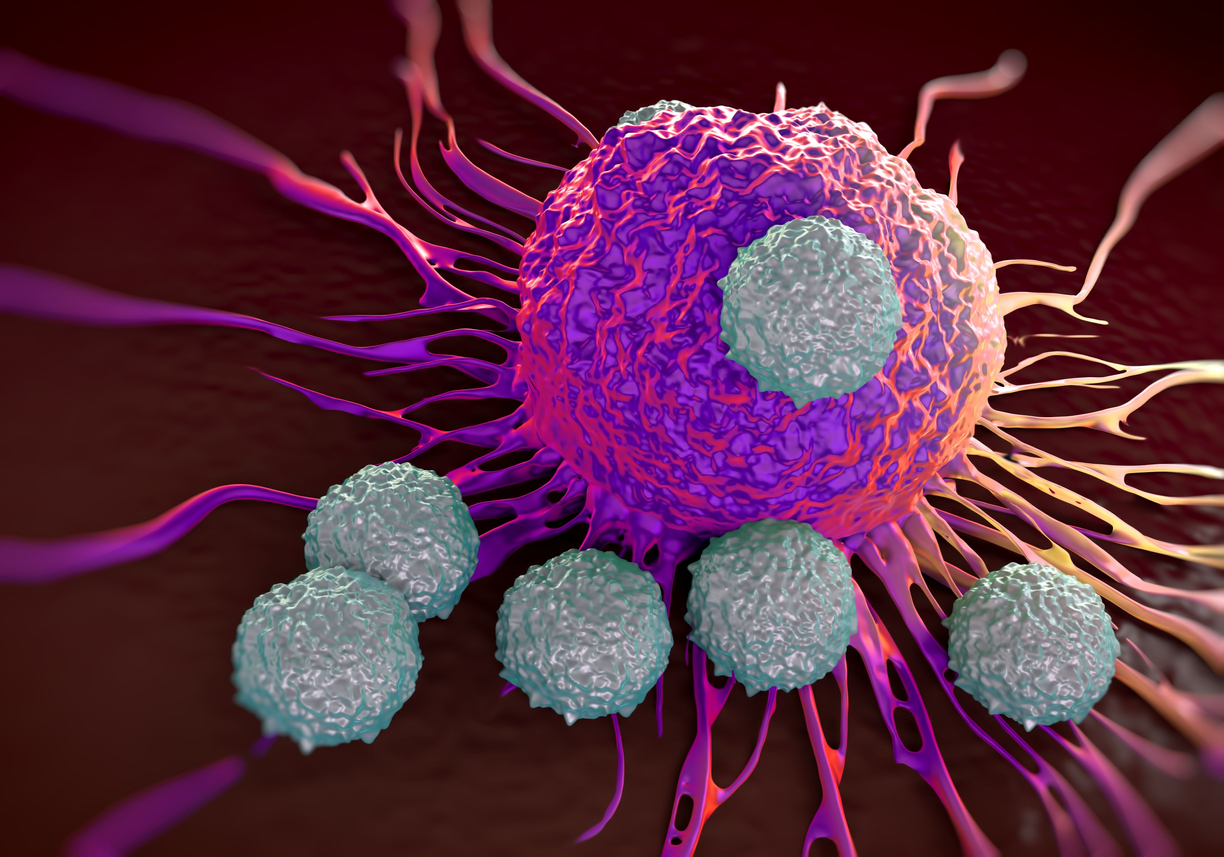
CAR T-cell therapy is a type of cancer cell and gene therapy where scientists remove patients’ T cells, add a laboratory-created protein receptor, and infuse the adapted cells back into the body. This protein receptor is called a “chimeric antigen receptor,” or CAR. Its intent is to help the T cells target cancer cells with a particular protein. A long-term goal is that the CAR T cells will replicate and create a “living drug” that continues to swat back any attempt by cancer to return.
The emerging therapy is approved by the U.S. Food and Drug Administration (FDA) for blood cancers like leukemia, lymphoma and multiple myeloma. Patients in early clinical trials have lived for 10 years thanks to a single infusion of CAR T cells.
There are a few concerns for using CAR T cells to battle solid tumors, like pancreatic cancer, lung cancer, glioblastoma and ovarian cancer. The lab-modified T cells become fatigued from interacting with resistant solid tumors. This makes the CAR T cells less effective.
CAR T cells also struggle to find the protein targets on solid tumors. Most exist within the cells rather than on the surface (like blood cancers).
These challenges can make CAR T-cell therapy less effective for some patients. In a few cases, the cells attack healthy tissue with the target protein more than cancer cells. CAR T-cell therapy can also cause a side effect called cytokine release syndrome, which is from an overstimulation of these immune cells.
SNIP CAR T cell offers more control for scientists

Dr. Mackall and her Stanford University colleagues conceived a CAR T-cell therapy called “SNIP CAR-T.” The CAR T cells are created with a block in signaling, which keeps the cells inactive. The scientists use a hepatitis C medication called grazoprevir, approved by the U.S. Food and Drug Administration, to override this inhibition and activate the cells. Without the drug, the SNIP CAR T cells are dormant.
The research team controlled the cells’ activity, providing a safety mechanism for anyone responding poorly to the cell and gene therapy. The CAR T cells also appear more effective against solid tumors because the cells received rest time each day as the effects of the daily hepatitis medication wore off, turning the cells from active to inactive.
In the SNIP CAR T-cell study, osteosarcoma (bone cancer) and medulloblastoma (brain cancer) were the two cancers tested. In many of the mice, the SNIP CAR T-cell therapy completely killed the cancer.
“When the SNIP CAR-T system with full dose grazoprevir is on, it’s full on. And when the grazoprevir is gone, it’s off. This is critical for patients who experience toxicity. We could turn the cells off and give the patient time to recover. Most other safety switches are designed to kill the CAR-T cells, or to turn them off forever. The patient might survive the treatment but still not be cured of their cancer.” — Crystal Mackall, MD, member of ACGT’s Scientific Advisory Council
Importance of Crystal Mackall, MD, and other cell and gene therapy researchers
Dr. Mackall holds several titles through her research at Stanford University:
- Founding Director of the Stanford Center for Cancer Cell Therapy
- Associate Director of the Stanford Cancer Institute
- Head of the Cancer Immunology and Immunotherapy Program
- Director of the Parker Institute for Cancer Immunotherapy at Stanford University
She’s also an ACGT Research Fellow, receiving a grant for her study of using a CAR T-cell therapy for pediatric neuroblastoma (nervous system cancer) and osteosarcoma. She recently helped a colleague develop a CAR T-cell therapy for a rare brain cancer called diffuse intrinsic pontine glioma, which mostly affects children.
Alliance for Cancer Gene Therapy funds researchers, like Dr. Mackall, who are using the power of science and technology to help the immune system more effectively target cancer. There is curative potential in cell and gene therapy, and discoveries like Dr. Mackall’s at Stanford move us closer to a future where cancer is not a deadly disease.
ACGT needs your help to continue funding this critical research. Please donate today to help us support the efforts of innovative scientists like Dr. Mackall, who are developing potentially life-saving cell and gene therapies and making the immune system more capable of fighting cancer. If you are not ready to donate, please sign up for ACGT’s email communications to get the latest news delivered to your inbox.
Page sources
- ‘Remote-controlled’ CAR-T cell therapy safer, more potent in Stanford mouse studies. Stanford Medicine. Retrieved from: https://med.stanford.edu/news/all-news/2022/05/snip-car-t-cell-therapy.html. Accessed: 06/08/2022.



