Standard of care chemotherapy and radiation have significant short and long-term side effects for patients as they kill healthy cells as well as cancer cells. Many patients describe these side effects as worse that the actual disease.
CAR T-cell therapy, while curative for certain blood cancers, comes with its own side effects, albeit ones potentially manageable to improve quality of life.
Chimeric antigen receptor (CAR) T-cell therapy, a type of cancer cell and gene therapy, is already significantly improving life expectancies for some people with blood cancer. Through the work of organizations like Alliance for Cancer Gene Therapy, the hope is to bring the same results to patients with solid tumors: pancreatic, ovarian, lung, and brain cancers, to name just a few.
One of the concerns many cancer patients have are side effects. “What are the possible or likely side effects?” is usually one of the first questions patients ask their physicians before starting a therapy.
Explaining CAR T-cell therapy
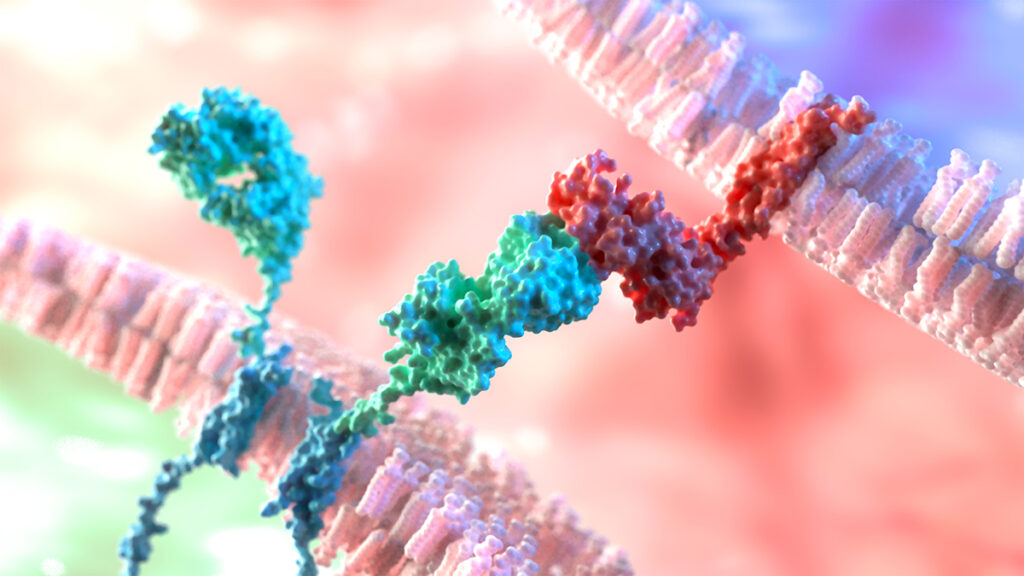
CAR T-cell therapy involves removing a patient’s T cells, adding RNA code to target cancer cells with specific biomarkers, and infusing them back into the patient’s bloodstream. This process of creating and administering CAR T cells – adding entirely new cells to the body – can lead to expected side effects.
Fortunately, non-profit organizations like Alliance for Cancer Gene Therapy continue to fund research programs to create stronger and safer CAR T cells. The Alliance funded the initial research by Carl June, MD, at the University of Pennsylvania, to advance the first successful CAR T cell therapies for blood cancers.
Alliance for Cancer Gene Therapy accomplished this feat in large part through donations from people like you – and the Alliance will continue to advance cell and gene therapy breakthroughs with your donation.
What is the main side effect of CAR T-cell therapy?
As the CAR T cells multiply, they release small proteins called cytokines into the blood. This release springs the immune system into action, but it can also cause a serious side effect called Cytokine Release Syndrome (CRS). Cytokine release syndrome is caused by a large, rapid release of cytokines into the blood from immune cells affected by CAR T-cell therapy and other immunotherapies.
Well-managed for most patients today, CRS was identified by Dr. Carl June during his treatment of acute lymphoblastic leukemia survivor Emily Whitehead. She was the first child treated with CAR T cells.
Most cases of CRS are mild, defined by discomfort and flu-like symptoms:
- Fever
- Fatigue
- Chills
- Nausea, with or without vomiting
- Headaches
- Dizziness
Other effects – like trouble breathing, low blood pressure, or a fast heartbeat – are more concerning. In severe cases of CRS, patients may need intensive care. Interestingly, the onset of CRS often indicates that the immune system is responding, a sign CAR T therapy is successfully fighting the cancer.
The severity of CRS is low, according to a multi-center study in the United States. The approved CAR T-cell therapy Yescarta (axicabtagene ciloleucel) was given to 275 patients with large B-cell lymphoma, a type of blood cancer. Only 7% of the patients had a grade 3 or grade 4 form or CRS, while 84% had grade 1 or grade 2 (mild) CRS. A small percentage (9%) didn’t experience CRS at all after their infusion of CAR T cells.
Despite this potential side effect, there are six CAR T-cell treatments approved by the U.S. Food and Drug Administration for certain blood cancers. The survival benefit and curative potential far outweighs the risk of side effects for types of leukemia, lymphoma and melanoma. Thanks to CAR T-cell treatment, some patients are deemed cured by their doctors.
Still, there is patient benefit to diminishing CRS from CAR T-cell therapy. Fortunately, there has been a lot of progress in making CAR T-cell therapy safer and more manageable for patients.
How can doctors control cytokine release syndrome after CAR T-cell therapy?
For years, doctors and patients managed CRS as part of the CAR T-cell process. Now it seems there may be additional ways to curtail the severe effects of this condition.
Three control methods have emerged from recent publications. They require more testing but indicate at least a possibility of preventing or treating cytokine release syndrome.
Arthritis medication diffuses CRS
Anakinra, an IL-1 inhibitor, is a medication for arthritis. Researchers at Memorial Sloan Kettering Cancer Center found another use: preventing serious cytokine release syndrome after CAR T-cell therapy.
IL-1 is a family of 11 cytokines responsible for producing inflammation in response to infections. Blocking this group of cytokines may control the severity of CRS.
Doctors gave anakinra to 31 patients with lymphoma. All of them received CD19 CAR T cells. There were no cases of grade 5 CRS. One patient had grade 4 CRS and one had grade 3 CRS.
Light-activated CAR T cells provide more control
Scientists at the University of Massachusetts Chan Medical School developed a nanoparticle to activate and control CAR T cells with light sensitivity. They found that the light-activated therapy caused decreased cytokine release and less damage to the body’s B cells.
The standard process for CAR T-cell therapy infuses cells back into the body with limited control of what the cells do afterward. Light activation provides an additional measure of supervision and direction, as doctors can selectively turn on the CAR T cells and limit how many are active in the immune system at any given time.
Disabling a CAR T-cell protein
Another option is to suppress Interferon gamma (IFNγ), a cytokine produced by CAR T cells. IFNy is one cause of CRS, and a team at Massachusetts General Hospital Cancer Center sought to suppress this particular cytokine to see if this prevents CRS.
Marcela Maus, MD, PhD, director of the center’s Cellular Immunology Program, said blocking or deleting IFNy didn’t stop anti-tumor activity. The CAR T cells remained effective against blood cancers and caused cytokine release syndrome less often.
“This could make CAR T cells an easier and more accessible therapy for patients.” — Marcela Maus, MD, PhD
Page sources
- Han lab developing light-activated immune cell therapy for cancers. UMass Chan Medical School. Retrieved from: https://www.umassmed.edu/news/news-archives/2021/12/han-lab-developing-light-activated-immune-cell-therapy-for-cancers/. Accessed: 12/29/2021.
- A Phase II Study of Prophylactic Anakinra to Prevent CRS and Neurotoxicity in Patients Receiving CD19 CAR T Cell Therapy for Relapsed or Refractory Lymphoma. ASH. Retrieved from: https://ash.confex.com/ash/2021/webprogram/Paper150431.html. Accessed: 12/29/2021.
- Blockade or deletion of IFNg reduces macrophage activation without compromising CAR-T function in hematologic malignancies. Blood Cancer Discovery. Retrieved from: https://bloodcancerdiscov.aacrjournals.org/content/early/2021/12/09/2643-3230.BCD-21-0181. Accessed: 12/29/2021.
- Severity of Cytokine Release Syndrome Influences Outcomes After Axicabtagene Ciloleucel for Large B-cell Lymphoma: Results from the US Lymphoma CAR-T Consortium. Clinical Lymphoma, Myeloma & Leukemia. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/35780055/. Accessed: 07/05/2022



