The success of cell and gene therapy for blood tumors was a monumental moment in cancer treatment. Eyes have turned now toward solid tumors.
Blood cancers and solid tumors, however, are quite different. Pancreatic, lung, ovarian, prostate and brain cancers pose challenges for cell and gene therapy.
Alliance for Cancer Gene Therapy lists three main challenges and ways scientists are overcoming them to use cell and gene therapy for solid tumors. After reading, please consider a gift to Alliance for Cancer Gene Therapy. Our non-profit organization provides important funding to cell and gene therapy researchers, who aim to overcome these challenges.
On-target, off-tumor toxicity
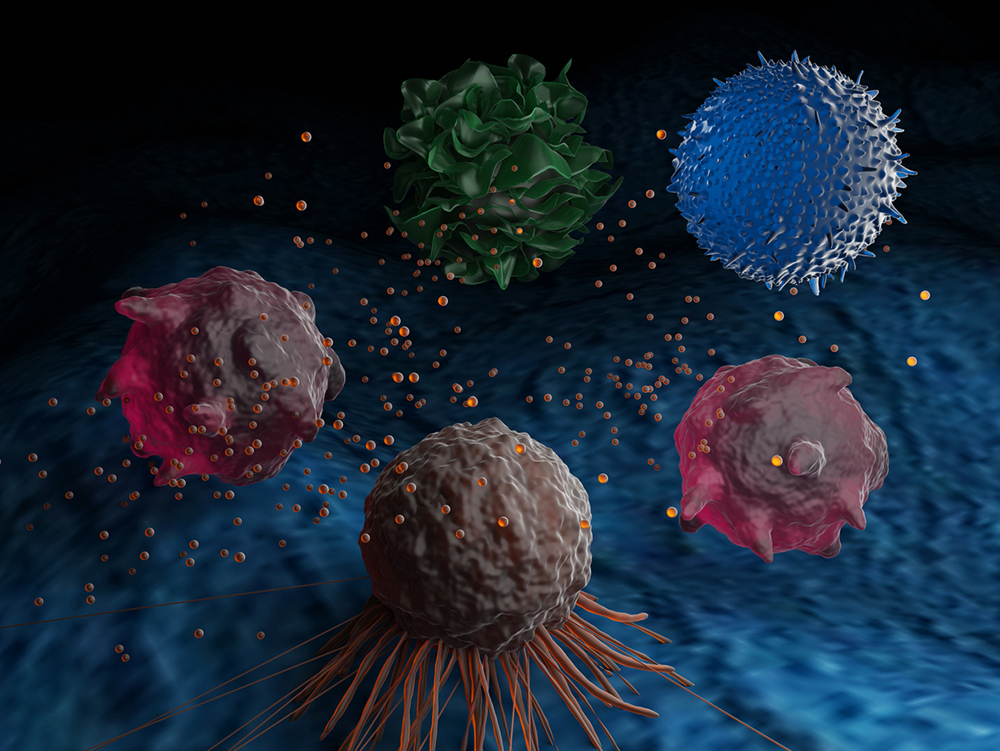
On-target, off-tumor toxicity means engineered immune cells are targeting healthy tissue with the same protein target. This is one of the challenges facing CAR T-cell therapy. CAR, the acronym for chimeric antigen receptor, adds a protein receptor to T cells to engineer them to target cancer cells expressing the target protein. A half dozen CAR T-cell therapies are approved for specific types of blood cancer like lymphoma, leukemia and myeloma.
The ideal target for CAR cell therapy is a protein expressed on cancer cells but not on normal tissue. Antigen selection is critical when creating CAR T cells or CAR NK (natural killer) cells.
Scientists can also direct the engineered immune cells to focus on cells with a high expression of the antigen and ignore healthy tissue with a low expression. This approach is called affinity tuning. A third option is to use two antigen targets – sometimes adding an engineered T-cell receptor – with the second differentiating between cancer cells and healthy tissue.
T-cell exhaustion
Solid tumors are stronger and more resistant to therapy. One explanation is that cancerous protein markets are inside the cells of solid tumors rather than on the surface like they are for blood tumors. Another is that many solid tumors are “cold,” and cold tumors have an immune-suppressing microenvironment with cells able to subdue the power of T cells. This means it requires more time and effort for T cells to reach their target.
The body’s natural T cells often tire out in this fight and become less effective as the battle continues. CAR T cells experience the same exhaustion. Exhausted CAR T cells produce lower amounts of immune-stimulating proteins, higher amounts of immune-suppressing proteins like PD-L1 and CTLA-4, and become less capable of infiltrating solid tumor cells.
One way around this stumbling block is to focus on genes that encode proteins linked to T-cell exhaustion. The National Cancer Institute reported two proteins, TOX and TOX2, as targets. Removing these two proteins from CAR T cells was one approach to diffusing exhaustion.
One of Alliance for Cancer Gene Therapy’s affiliated scientists found a potential avenue to address T-cell exhaustion. Carl June, MD, a Scientific Advisory Council member and Research Fellow of the Alliance, reported ID3 and SOX4 as two immune-suppressing proteins prevalent in pancreatic cancer. Dr. June and his team at Penn Medicine’s Abramson Cancer Center believe these two proteins are offenders of T-cell exhaustion – and neutralizing them may help CAR T cells fight pancreatic cancer cells.
Blood-brain barrier
The blood-brain barrier is an obstacle specific to brain cancers, like glioblastoma or glioma. Around 25,000 people in the United States are diagnosed with brain cancer each year.
The blood-brain barrier is a wall of endothelial cells that separates the bloodstream from the region where the brain resides. The purpose of the barrier is to block any toxins in the blood from reaching the central nervous system and supply the brain with nutrients.
While the barrier intends to protect the brain, it is a major obstacle for the immune system when cancer has formed in the organ. T cells and other immune cells travel throughout the body using blood vessels and lymph nodes. The barrier blocks these cells from reaching the central nervous system.
CAR T cells are often infused into the patients’ blood, meaning they also face the same dilemma when trying to reach the brain.
One way of bypassing the blood-brain barrier is injecting cell and gene therapy directly into the brain region. This is called delivering therapy intracranially. Christine Brown, PhD, a member of the Alliance for Cancer Gene Therapy Scientific Advisory Council, reported success using this method in a phase 1 CAR T-cell trial for relapsed glioblastoma. Survival rates for the patients surpassed the usual average survival for relapsed glioblastoma.



