The premise of T-cell therapy is engineering T cells to attack cancer cells with a specific protein. The evolution of this cancer cell and gene therapy is to be selective about the protein targeted.
Researchers at multiple cancer centers and medical universities have identified a protein receptor capable of strengthening T-cell therapy against cancer. The scientists discovered that adding an IL-9 receptor makes the T cells strong enough to fight cancer without needing chemotherapy beforehand.
Alliance for Cancer Gene Therapy put together an overview of T-cell therapy, what the IL-9 receptor is, and why this receptor holds potential as a target of cell and gene therapy.
What is T-cell therapy?
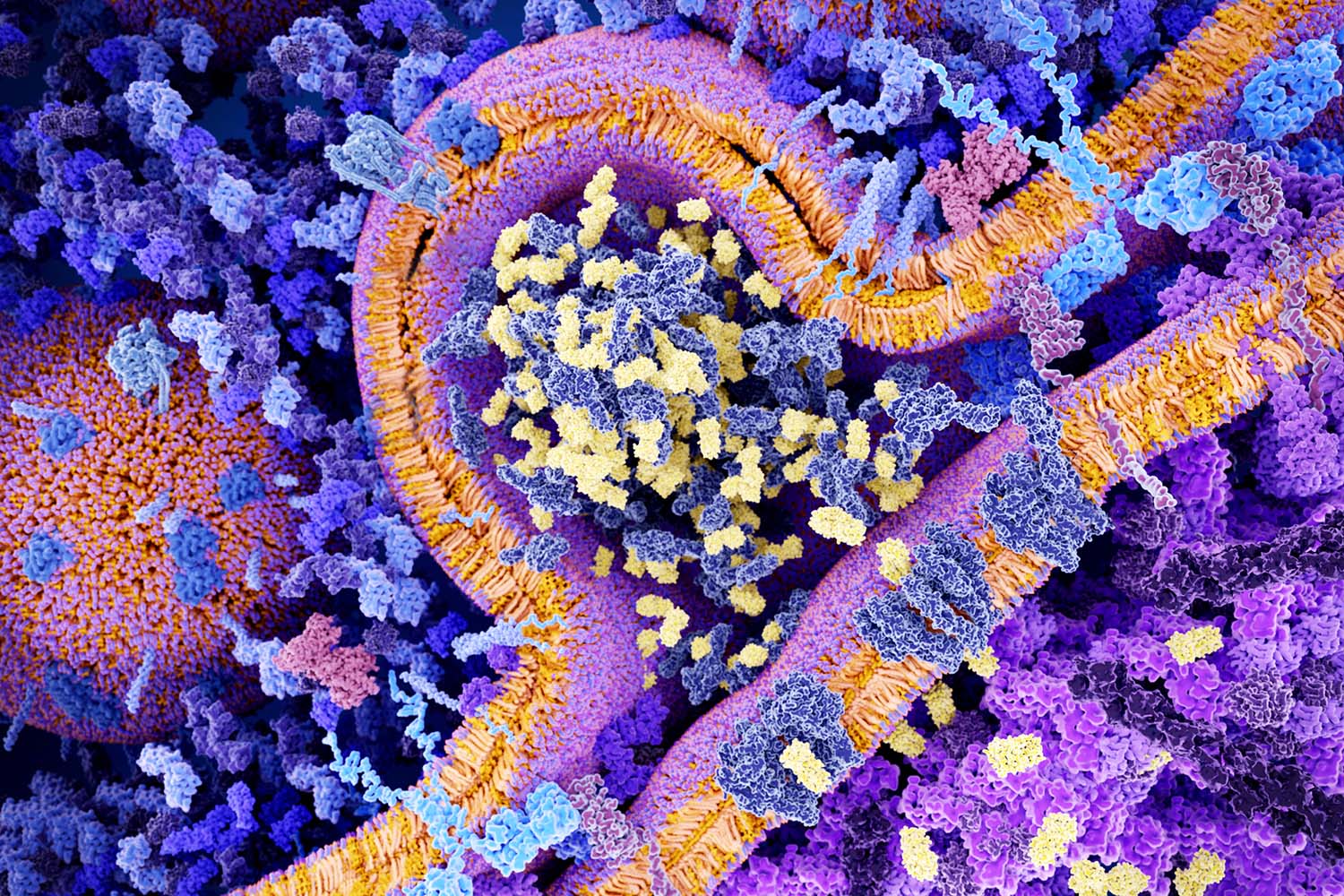
T-cell therapy is one of many types of cancer cell and gene therapy. There are different types of T-cell therapy, one being CAR T-cell therapy.
CAR T-cell therapy removes a patient’s T cells, adds a protein receptor (chimeric antigen receptor, or CAR), and adds the enhanced T cells back into the body. The current FDA approvals of CAR T-cell therapy for various blood cancers require chemotherapy first before patients can try the cell and gene therapy.
Another type of T-cell therapy is engineered T-cell receptors. These enhanced T cells look for proteins broken down in the major histocompatibility complex, which presents fragments of proteins to T cells. Engineered T cells are directed to look for specific proteins found in the complex.
What is IL-9?
IL-9 is a protein created by immune cells. It stimulates cell replication and helps keep cells alive. It’s an important protein for cellular balance but can cause cancer cells to live far past their usual life cycle.
There are other proteins with a similar name (IL-2, IL-7 and others). However, IL-9 seems to have the most potential as a target for cell and gene therapy.
Why is IL-9 a protein target for cell and gene therapy?
IL-9 could be used as a second target for T cells. Scientists can add two protein receptors to the cells, one for a primary protein and another for IL-9. This process would involve creating a synthetic form of the protein to signal and stimulate the T cells to grow and multiply at faster rates.
Since this synthetic signal doesn’t apply to ordinary T cells, only the engineered ones will multiply. This effect may do away with the need for preconditioning chemotherapy.
Using IL-9 against pancreatic cancer and melanoma
Research teams at three medical institutions – UCLA, Stanford University and the University of Pennsylvania – tested IL-9 as a second protein receptor target for T-cell therapy. CAR T-cell therapy was tested on human and mouse models of melanoma (a skin cancer). Engineered T-cell receptor therapy was tested on human and mouse models of pancreatic cancer.
In both types of cell and gene therapies and both types of cancer, the presence of a synthetic IL-9 signal on the T cells was effective. Stimulated T cells engineered with a synthetic IL-9 receptor were better than normal T cells in killing these two cancers. The study authors said T cells stimulated with IL-9 were better at reaching the tumor and surviving the hostile tumor microenvironment surrounding solid tumors like pancreatic cancer.
If you’d like more news about cell and gene therapy – including specifics about how this field of science treats cancer at the cellular and protein level – sign up for our monthly email newsletter. This offering provides a list of the most recent articles published on Alliance for Cancer Gene Therapy, plus industry news in cell and gene therapy.
Page sources
- New study with UCLA researchers finds improvements to T-cell therapy for cancer. The Daily Bruin. Retrieved from: https://dailybruin.com/2022/08/28/new-study-with-ucla-researchers-finds-improvements-to-t-cell-therapy-for-cancer. Accessed: 08/30/2022.



