
What if cancer patients could receive CAR T cells through a surgical implant rather than the multi-week process creating the cells often takes?
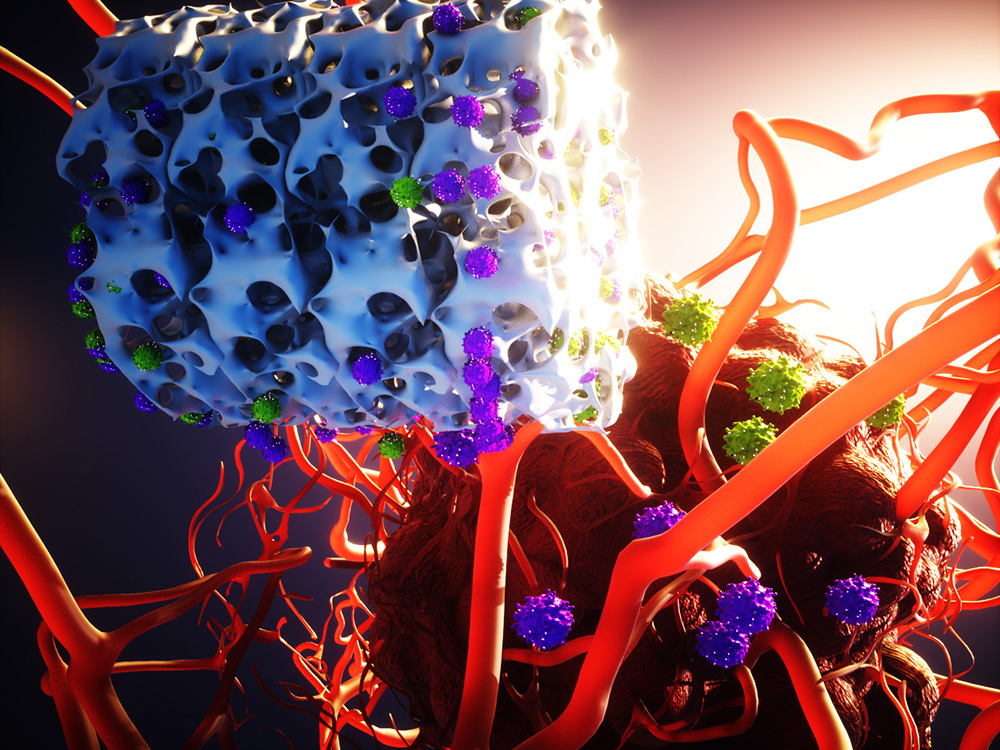
This theory is being explored by researchers at University of North Carolina (UNC) and North Carolina State University (NC State), who are working in tandem to create an “implantable biotechnology” that produces and delivers CAR T cells to attack cancerous cells. The hope is the implant process is quicker – without sacrificing effectiveness – than the traditional method.
Researchers at the two universities tested their creation on mice with lymphoma, a type of blood cancer with multiple CAR T-cell approvals from the U.S. Food and Drug Administration. The results indicate a shorter turnaround time for delivering the CAR T cells and stronger cells for the patient’s immune system to fight the tumor.
This is not the first piece of news involving an attempt to quicken the CAR T-cell therapy process. Scientists at Penn Medicine’s Abramson Cancer Center believe they have a method to produce powerful CAR T cells in under 24 hours.
Alliance for Cancer Gene Therapy (ACGT) similarly reported on Penn Medicine’s potential advancement. ACGT’s mission is to support cancer cell and gene therapies – like CAR T-cell therapy – by funding research programs and raising awareness of their potential to the general cancer community. Learn more about Alliance for Cancer Gene Therapy’s mission, why our organization exists and how we use your donation to support potentially life-saving cancer studies.
How are CAR T cells created?
CAR T-cell therapy is a type of cell and gene therapy receiving a large amount of attention and resources as a potential treatment for many types of cancer. The creation of CAR T cells involves a multi-step process spanning at least a week, sometimes multiple weeks.
The steps are:
- Doctors draw a patient’s blood and separate the T cells from the blood
- The T cells are sent from the hospital to a laboratory
- Scientists expose the T cells to antibodies to activate, or wake up, the cells
- Once activated, the T cells receive the chimeric antigen receptor (CAR) gene, via a virus, with directions for seeking cancer cells with a specific biomarker
- The reprogrammed cells replicate to create a larger population
- The CAR T cells are returned to the hospital and infused into the patient
The longest steps involve the work in the laboratory to expose the T cells to antibodies, deliver the CAR gene via a virus, and multiply the engineered T cells into a cancer-fighting army.
“Reducing the manufacturing time is even more critical for patients with rapidly progressing disease.” — Pritha Agarwalla, postdoctoral researcher at UNC School of Medicine
What do UNC and NC State researchers propose?
Scientists at the two universities created a biotechnology called MASTER, or “Multifunctional Alginate Scaffolds for T cell Engineering and Release.” The article on the UNC School of Medicine website describes MASTER as a sponge-like material “with the look and feel of a mini marshmallow.”
The fascinating element is that most of the laboratory work done in the conventional CAR T-cell creation process occurs within MASTER. Researchers isolated T cells from blood – like they would in the conventional approach – but, instead of sending them to the lab, mixed them with the virus. The mixture is added to MASTER, which absorbs it. MASTER already has the necessary antibodies for T-cell activation and the necessary proteins for CAR T-cell replication.
In testing using mice, the biotechnology was surgically implanted. The technology must still be developed through further early testing before considering it for patients.
“Our MASTER technology takes the cumbersome and time-consuming activation, reprogramming and expansion steps and performs them inside the patient. This transforms the multi-week process into a single-day procedure.” — Pritha Agarwalla, postdoctoral researcher at UNC School of Medicine
Testing the MASTER biotechnology against conventionally created CAR T cells
MASTER significantly reduced the development time for CAR T-cell therapy. Did it create and deliver effective CAR T cells, though?
The scientists compared the MASTER CAR T cells with conventionally created and intravenously delivered engineered cells. The result was healthier cells from the MASTER biotechnology, since there is less manipulation and less time outside of the patient’s body. One of the measurements for this conclusion was T-cell exhaustion, a biological phenomenon where T cells lose their strength and endurance from attacking tumors.
“The end result is that the mice that received CAR-T cell treatment via MASTER were far better at fighting off tumors than mice that received conventional CAR-T cell treatment,” Agarwalla said in the UNC School of Medicine article.
While lymphoma was the focus of the research, scientists at the two universities plan to test MASTER on solid tumors such as pancreatic cancer and brain tumors. CAR T-cell therapy is growing support for blood cancers, but it has not yet worked consistently enough for solid tumors. Scientists across the country are exploring ways to develop effective CAR T cells to treat complex and challenging solid tumors.
Page sources
- Implant Churns Out CAR-T Cells to Combat Cancer in Animal Models. UNC School of Medicine. Retrieved from: https://news.unchealthcare.org/2022/03/implant-churns-out-car-t-cells-to-combat-cancer-in-animal-models/. Accessed: 04/06/2022.



